Understanding the Link Between Gut Health and Chronic Pain: A Functional Medicine Approach
The Frustrating Cycle of Chronic Pain—and a Missing Piece
If you've been living with chronic back pain, persistent neck stiffness, or aching joints that just won't quit, you know the exhaustion that comes with it. You've tried medications, adjustments, even changed your routines—yet the pain lingers. What if part of the answer isn't just in your spine or joints, but in a place you'd never think to look: your gut?
Emerging research reveals a powerful connection between digestive health and chronic pain. For many adults in Stuart, Florida and the surrounding Treasure Coast communities, addressing gut health through a functional medicine lens is opening new doors to relief and restored quality of life.
What Does "Gut Health" Really Mean?

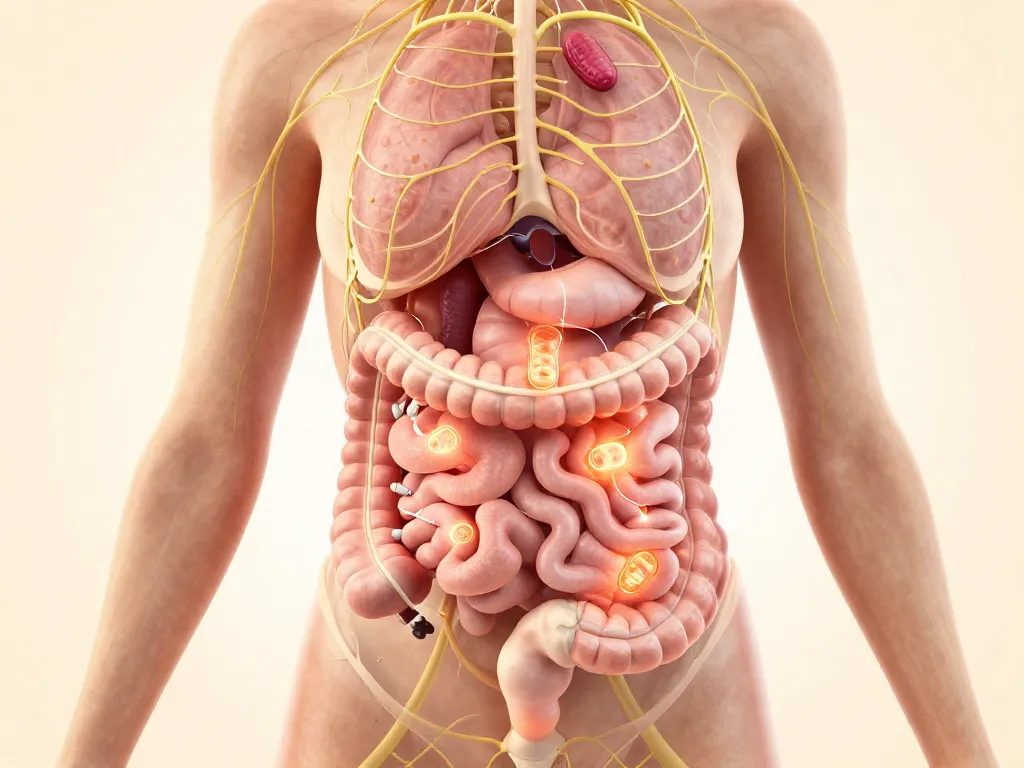
When we talk about "gut health," we're referring to three key things:
Your Microbiome:The trillions of bacteria, fungi, and other microorganisms living in your digestive tract. When balanced, they help digest food, produce vitamins, and keep your immune system in check. When out of balance (called dysbiosis), they can trigger widespread problems.
Your Gut Barrier:The lining of your intestines acts like a selective gatekeeper, letting nutrients in while keeping toxins and undigested particles out. When this barrier becomes compromised (often called "leaky gut" or increased intestinal permeability), unwanted substances can slip into your bloodstream.
Your Digestion:How well you break down and absorb nutrients from food directly affects energy, tissue repair, and your body's ability to manage inflammation.
All three work together—and when they're not working well, the effects can reach far beyond your stomach.
How Can Gut Problems Contribute to Chronic Pain?
The gut-pain connection might sound surprising, but it makes sense once you understand the pathways involved:
Inflammation Spreads Beyond the Gut
When your gut barrier is compromised or your microbiome is imbalanced, inflammatory signals can increase throughout your body. Research published by theNational Institutes of Healthsuggests that systemic inflammation is a common thread linking digestive dysfunction to musculoskeletal pain¹. Inflammatory molecules called cytokines can travel through the bloodstream, affecting joints, muscles, and nerves far from the gut itself.
Your Immune System Gets Confused
About 70% of your immune system resides in and around your gut. When the gut environment is disrupted, your immune system may become overactive or misdirected, sometimes attacking your own tissues. Some studies have found associations between altered gut bacteria and conditions like rheumatoid arthritis and fibromyalgia².
Nutrient Deficiencies Develop
Chronic digestive issues can impair your ability to absorb key nutrients—magnesium, vitamin D, B vitamins, and omega-3 fatty acids—that are essential for nerve health, muscle function, and controlling inflammation. Low nutrient status may worsen pain sensitivity and slow healing.
The Gut-Brain-Pain Axis
Your gut and brain communicate constantly via the vagus nerve and chemical messengers. An unhappy gut can influence stress hormones, sleep quality, and even how your nervous system processes pain signals. This bidirectional relationship means that gut distress can amplify pain perception, while chronic pain and stress can further harm gut health³.
Common Signs Your Gut and Pain May Be Connected
Not everyone with chronic pain has obvious digestive symptoms, but many do experience overlapping issues such as:
Frequent bloating or gas
Irregular bowel movements (constipation, diarrhea, or both)
Food sensitivities or reactions
Persistent fatigue, even after rest
Brain fog or difficulty concentrating
Skin issues like eczema or rashes
Important note:These symptoms are nonspecific and can occur for many reasons. They don't automatically mean you have a gut issue, but they're clues worth exploring—especially if you've struggled with pain that doesn't fully respond to conventional treatments.
The Functional Medicine Approach: Looking for Root Causes

Unlike conventional care that often focuses on symptom management, Functional Medicine digs deeper. The goal is to understand why you're experiencing pain, not just what hurts.
A Thorough Health History
Your practitioner will ask detailed questions about:
When your pain started and what makes it better or worse
Your digestive patterns and diet
Stress levels, sleep quality, and emotional health
Past infections, antibiotic use, or major life events
Family history of autoimmune or inflammatory conditions
Lab Testing That May Be Considered
Depending on your unique situation, functional medicine providers may explore tests such as:
Comprehensive stool analysis (to assess microbiome diversity and inflammation markers)
Food sensitivity panels
Inflammatory markers (CRP, ESR)
Nutrient levels (vitamin D, B12, magnesium, omega-3 index)
Gut permeability assessments
These are examples only; not every patient needs every test. Your provider will recommend what's appropriate for you.
Personalized, Integrative Plans
Based on findings, your care plan may blend dietary adjustments, targeted supplements, stress management techniques, and therapies like Chiropractic Care,Spinal Decompression,Shockwave Therapy, or Red Light Therapy—all designed to address the interconnected factors driving your pain.
Safe, Practical Steps You Can Start Today
You don't need expensive tests or prescriptions to begin supporting your gut health. Here are evidence-informed, low-risk strategies you can try at home:
1. Focus on Whole, Colorful Foods
Fill your plate with vegetables, fruits, lean proteins, and healthy fats. These provide fiber and phytonutrients that feed beneficial gut bacteria.
2. Increase Fiber Gradually
Aim for 25–35 grams of fiber daily from sources like leafy greens, berries, beans, and oats. Fiber supports regular digestion and helps reduce inflammation⁴.
3. Stay Hydrated
Water is essential for digestion and nutrient transport. Aim for at least 8 cups per day, more if you're active or live in Florida's warm climate.
4. Prioritize Sleep and Stress Management
Poor sleep and chronic stress harm both gut health and pain tolerance. Simple practices—deep breathing, short walks, or 10 minutes of stretching—can make a real difference.
5. Move Gently and Consistently
Low-impact activities like walking, swimming, or yoga support digestion, circulation, and mood without aggravating pain.
6. Consider Probiotic-Rich Foods
Yogurt, kefir, sauerkraut, and kimchi may help diversify your gut microbiome. Start small to see how your body responds.
Start small: Pick one or two changes this week. Progress matters more than perfection.
When Should You Seek Professional Help?

You should reach out to a qualified provider if you experience:
Red-flag symptoms: Unexplained weight loss, blood in stool, severe abdominal pain, or fever
Chronic symptoms that persist: Pain, digestive issues, or fatigue lasting more than a few months despite self-care
Impact on daily life: When symptoms interfere with work, family, sleep, or activities you love
Desire for a personalized plan: If you've tried conventional treatments without lasting relief and want a deeper investigation
Don't wait until pain controls your life. Early, proactive care often leads to better outcomes.
How Coastal Medical and Wellness Can Help You
At Coastal Medical and Wellness, serving Stuart, Palm City, Jensen Beach, and surrounding communities on Florida's Treasure Coast, we specialize in finding the root causes of chronic pain—not just masking symptoms.
What to Expect at Your Initial Visit:
Comprehensive consultation: We'll listen to your full health story and understand your goals.
Personalized assessment: We may recommend functional lab work, physical exams, or advanced imaging as appropriate.
Integrative care plan: Drawing from functional medicine, chiropractic, regenerative therapies, and lifestyle coaching, we'll build a plan tailored toyourbody andyourlife.
Ongoing support: Healing takes time. We'll walk with you every step of the way, adjusting your plan as you progress.
Whether your pain stems from inflammation, structural issues, nutrient imbalances, or a combination of factors, our team is here to help you reclaim your health and vitality.
Take the First Step Toward Relief
You've lived with chronic pain long enough. If you're curious whether gut health could be part of your pain puzzle, we invite you to explore a functional medicine approach.
📞 Call Coastal Medical and Wellness today at 772-286-5277 to schedule your consultation.
Let's work together to uncover the root causes, restore balance, and help you feel like yourself again.
About Coastal Medical and Wellness
Coastal Medical and Wellness is a patient-centered integrative clinic in Stuart, Florida, combining the latest in functional medicine, chiropractic care, and regenerative therapies. Our experienced team is dedicated to helping adults overcome chronic pain, inflammation, and fatigue through personalized, evidence-informed care. We proudly serve families throughout Martin County and beyond.
Medical Disclaimer
This blog post is for educational purposes only and does not constitute medical advice, diagnosis, or treatment. Always consult with a qualified healthcare provider before making changes to your diet, exercise, or treatment plan, especially if you have underlying health conditions or are taking medications. Individual results may vary.
Frequently Asked Questions (FAQs)
1. Can poor gut health really cause back pain?
While gut health alone may not "cause" back pain, research suggests that gut inflammation and immune dysregulation can contribute to systemic inflammation, which may worsen musculoskeletal pain. Addressing gut issues is one piece of a comprehensive pain management strategy.
2. What is functional medicine, and how is it different from regular medicine?
Functional medicine focuses on identifying and addressing root causes of illness rather than only treating symptoms. It uses detailed health histories, advanced lab testing, and personalized lifestyle and nutrition plans alongside conventional and integrative therapies.
3. How long does it take to see improvements in pain after addressing gut health?
Every person is different. Some notice changes within a few weeks, while others may need several months of consistent care. Factors like the severity of dysbiosis, adherence to the care plan, and overall health all play a role.
4. Do I need special tests to know if my gut is affecting my pain?
Not always. A thorough health history and trial of gut-supportive strategies can be informative. However, targeted lab work (stool analysis, inflammatory markers, nutrient testing) can provide valuable insights and help personalize your treatment.
5. Is functional medicine covered by insurance?
Coverage varies by plan. Some functional medicine services may be covered, while specialty lab tests or supplements typically are not. Our team at Coastal Medical and Wellness can discuss payment options and provide documentation for possible reimbursement during your consultation.
References
National Institutes of Health. "The Role of the Gut Microbiome in Chronic Pain."NIH News in Health, 2023.nih.gov
Mu, Q., Kirby, J., Reilly, C. M., & Luo, X. M. "Leaky Gut As a Danger Signal for Autoimmune Diseases."Frontiers in Immunology, 2017.frontiersin.org
Mayer, E. A., Nance, K., & Chen, S. "The Gut-Brain Axis."Annual Review of Medicine, 2022.annualreviews.org
Harvard T.H. Chan School of Public Health. "Fiber and Inflammation."The Nutrition Source, 2024.hsph.harvard.edu
Cleveland Clinic. "How Your Gut Health Affects Your Whole Body."Health Essentials, 2023.clevelandclinic.org
